BY DR. EVA HAMRUD: I am a bioinformatician with a primary research interest in stem cell biology. I am also passionate about all areas of scientific research and their communication.
Measles, the MMR vaccine and Misinformation
In 2000, the U.S. declared measles eliminated—meaning no sustained transmission for a year in the presence of strong surveillance. Yet, as of March this year, two deaths and 483 cases have already been reported. This resurgence is not due to a more virulent virus but rather declining vaccination rates. Let’s explore the science of measles, the MMR vaccine, and misinformation.
What is measles?
Measles, described as early as 900 AD, causes fever, cough, runny nose, conjunctivitis and a distinctive rash. Complications occur in 1 in 5 unvaccinated cases in the U.S., leading to pneumonia, encephalitis, and in some cases death – particularly in infants, malnourished children and the immunocompromised.
Caused by a single-stranded, RNA virus, measles spreads through airborne droplets released during coughing and sneezing. The virus attacks immune cells, leading to immunosuppression which increases susceptibility to secondary infections, some of which can be life-threatening.
With an R₀ of 12-18, measles is one of the most contagious diseases, as a single infected person can spread the virus to 12 to 18 others in a fully susceptible population. Controlling outbreaks is particularly challenging because patients are highly contagious for four days before and after the rash appears.

What is the treatment for measles?
There is no antiviral treatment for measles – care is usually supportive, such as keeping the patient hydrated and controlling fever. Vitamin A is beneficial for malnourished children, but there is no evidence that it lowers the risk of contracting measles.
How was the measles vaccine developed?
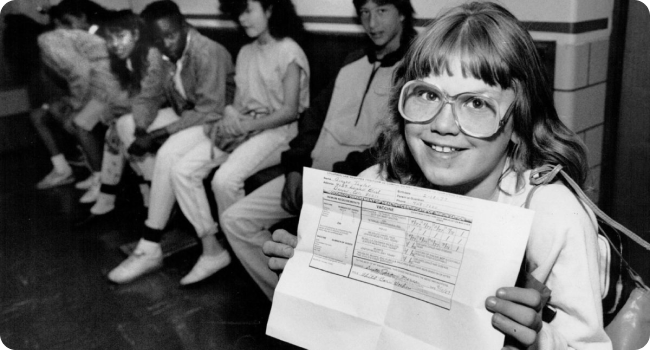
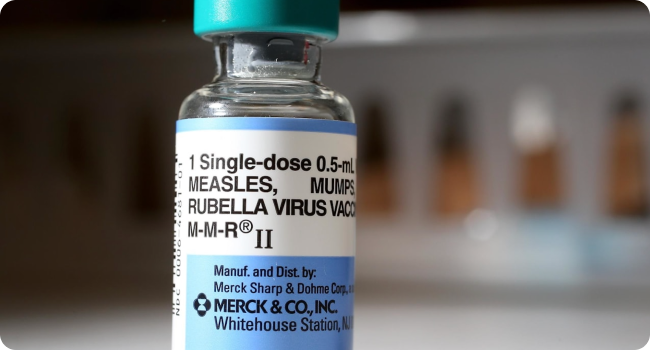
In 1954, American physician Dr. Thomas Peebles isolated the measles virus from an infected schoolchild, which was used to create the first vaccine against measles in 1963. This vaccine, along with all measles vaccines used since, was a ‘live-attenuated’ vaccine, meaning the virus is weakened so it triggers an immune response without causing disease. Although effective, the original measles vaccine had strong side effects, so was further refined by Dr Maurice Hilleman by passing it through chick embryos 40 times to further weaken it. In 1971 Dr Hilleman combined the measles vaccine with those for mumps and rubella, creating the MMR vaccine.
Why do we use the combined MMR vaccine rather than each vaccine separately?
After the development of the MMR vaccine in the 1970s, there was a large USA public health campaign to eradicate measles from the country. Part of the success of the campaign can be attributed to the streamlined immunisation programmes which used combined vaccines like MMR to reduce the number of doctor visits required for each child. Combination vaccines have been shown to save time and money for parents, reduce trauma for children, and ensure children receive their vaccinations in a timely manner and therefore avoid getting infected with potentially life-threatening diseases.
Is the MMR vaccine effective?
Before 1963, almost all children in the US developed measles before they turned 15. Two MMR doses provide 97% protection against measles. Among 2025’s cases, 97% of these were unvaccinated or had unknown vaccination status, and both fatalities were in unvaccinated individuals.
Epidemiological studies looking at the outbreaks of measles in the USA since its elimination in 2000 have found that outbreaks occur in areas of low vaccination coverage. For example, of the 7 biggest outbreaks between 2001 to 2019, 5 were in “known undervaccinated, close-knit communities” and 79% to 100% of cases were in unvaccinated people or those with unknown vaccine status.
What are the current measles vaccination guidelines and why?
Measles is one of the most contagious diseases, requiring an exceptionally high threshold for community protection compared to other diseases. Vaccination coverage of 93% to 95% is needed to achieve sufficient community immunity and prevent outbreaks.
The WHO recommends administering the first MMR dose at 9-15 months and the second at 4-6 years to boost immunity. Around 12 months is considered the ideal time for the first dose because maternal antibodies, which pass from mother to baby and provide early protection, begin to wane at this age, leaving the child more vulnerable to infection.
What are the vaccination stats?
Around 90-92% of children born between 2011 and 2021 in the U.S. have received at least 1 MMR jab, not hitting the 95% threshold to prevent endemic outbreaks of the disease. More importantly, vaccine coverage is not uniform. A analysing data from the CDC from 2009 to 2017 found that regions with high nonmedical exemptions to vaccination have very low MMR vaccine coverage, and therefore are the most vulnerable communities to measles outbreaks.
Vaccination rates do not appear to be increasing. Global vaccination coverage dropped during and after the COVID-19 pandemic, with measles vaccine coverage dropping from 86% in 2019 to 81% in 2021

Why do some people not get the MMR vaccine?
The drop in vaccination coverage for measles has been widely attributed to the spread of misinformation. Vaccine hesitancy has grown since the COVID-19 pandemic, but anti-vaccine activism has existed as long as vaccines have. One of the most damaging misinformation incidents was a paper published in 1998 linking the MMR vaccine to autism in 12 children. Despite investigations finding that all 12 of the children’s cases included falsified data, and that the author, British doctor Andrew Wakefield (who is now banned from practicing) secretly received financial incentives to discredit the MMR vaccine, the widespread media coverage of the case resulted in many parents becoming suspicious of the MMR vaccine.
Vaccine hesitancy is determined by contextual influences like the media and public figures as well as group influences such as family and friends. Unfortunately, online anti-vaccine movements, particularly on social media, have been found to use emotionally charged negative messaging to fuel vaccine hesitancy. As a result, a systematic review on parental attitudes to measles vaccination in Europe published in 2020 found that vaccine hesitancy was mainly due to concerns on vaccine safety and effectiveness, and their perceived risk of measles severity and prevalence.

What are the facts on MMR vaccination safety?
Despite claims made by many anti-vaccination misinformation sources, there is an overwhelming body of evidence in support of the safety of the MMR vaccine. Like all medical interventions, reporting of adverse events from the MMR vaccines are highly encouraged and this data is collated for analysis. A study of these adverse event databases, which includes anaphylaxis, seizures and other problems, found that there was no disproportionate reporting of adverse effects associated with MMR as compared to other vaccines over 30 years from 1989 to 2019. The most common side effects from the MMR vaccine include a sore arm, fever and a mild rash.
There have been no scientific publications to suggest that there is any benefit, either in safety or efficacy, to separating the three vaccines used in the MMR.
Fifty Years of MMR: Triumph and Challenge
After more than five decades of widespread use, the MMR vaccine has proven to be one of the greatest successes in public health history. With over 97% effectiveness against measles when properly administered and an exceptional safety record confirmed through decades of rigorous monitoring, the vaccine has saved millions of lives worldwide. The scientific and epidemiological evidence overwhelmingly supports its continued use. However, despite this remarkable achievement, declining vaccination rates driven by misinformation and parental hesitancy have become the primary obstacle to maintaining measles elimination. As recent outbreaks demonstrate, the science remains clear: high vaccination coverage is the only effective strategy to protect communities from this highly contagious and potentially serious disease. The current resurgence of measles represents not a failure of the vaccine but rather a failure to effectively communicate its proven benefits and counter the spread of misinformation.
Ask Consensus
🦠What is the reason for the recent measles outbreaks in the U.S.? 💉Is the MMR vaccine effective? 😷Is the MMR vaccine safe? 🧑🔬Why are MMR vaccination levels dropping?REFERENCES
Introduction
PAHO (WHO) page on measles
Official definition of disease ‘elimination’
BBC news article on recent measles deaths
CDC measles outbreak statistics (updated weekly)
What is measles
Article about the first book smallpox and measles
CDC measles factsheet
Book ‘Measles’ by Kondamudi and Waymack
Systematic review of the basic reproductive number of measles published in the Lancet
NHS measles factsheet
What is the treatment of measles
Research article on vitamin A and measles published in the International Journal of Epidemiology
The Conversation article on vitamin A and measles
How was the measles vaccine developed
History of Vaccine resource from the College of Physcians of Philadelphia
WHO article on history of measles vaccination
Fact sheet on vaccine types from US Department of Health and Human Services
Why do we use the combined MMR vaccine rather than each vaccine separately
Research article on Measles and the Modern History of Vaccination published in Sage Journals
CDC factsheet on vaccine safety
Is the MMR vaccine effective
CDC factsheet on history of measles
CDC factsheet on measles vaccination
Research article on maintenance of measles elimination status in the US published in Clinical Infectious Diseases
What are the current measles vaccination guidelines and why
WHO measles factsheet
What are the vaccination stats
CDC ‘ChildVaxView’ database on children vaccination rates in the U.S.
Research article on antivaccine movement in U.S. published in PLOS Medicine
Our World in Data page on vaccination rates
Why do some people not get the MMR vaccine
Research article on vaccine hesitancy published in Vaccines journal
Editorial on Wakefield’s article being fraudulent published in the British Medical Journal
Editorial on vaccine hesitancy published in Nature Immunology
Research article on antivaccine campaign strategies published in Nature
Systematic review on parental attitudes to vaccination published in Journal of Epidemiology and Global Health
What are the facts on MMR vaccination safety
Research article on MMR vaccine safety published in British Medical Journal
Research article on MMR vaccine adverse effects published in Open Forum Infectious Diseases
