This post was written with Consensus AI Academic Search Engine – please read our Disclaimer at the end of this article. Ulcerative colitis (UC) is a chronic inflammatory bowel disease characterized by continuous mucosal inflammation starting in the rectum and extending proximally. The disease presents with symptoms such as bloody diarrhea, abdominal pain, urgency, and tenesmus, and can have extraintestinal manifestations6 8. Understanding the complications and prognosis of UC is crucial for optimizing patient management and improving outcomes.
Complications of Ulcerative Colitis
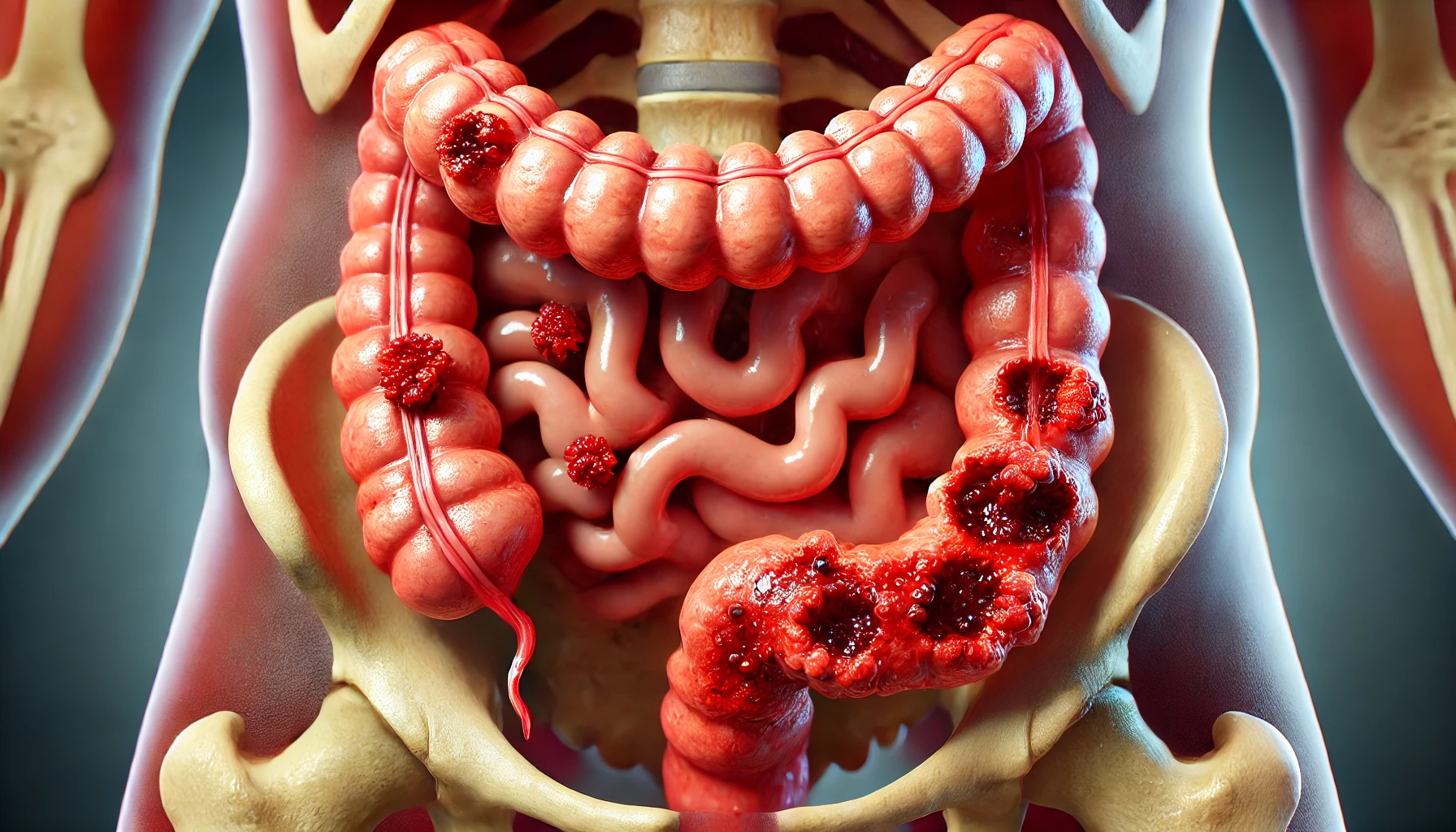
UC is associated with a variety of complications, which can be categorized into local and systemic complications. Local complications include severe colitis, toxic megacolon, and colorectal cancer, while systemic complications can affect distant parts of the body, such as the liver and skin3 8.
Local Complications
- Severe Colitis and Toxic Megacolon: Acute severe colitis (ASC) is a critical complication that can lead to toxic megacolon, a life-threatening condition requiring immediate medical intervention. Disease severity at onset and hypoalbuminemia are predictors of ASC1.
- Colorectal Cancer: Patients with UC are at an increased risk of developing colorectal cancer, particularly those with longstanding colitis, concomitant primary sclerosing cholangitis (PSC), and extensive disease1 7. The cumulative risk of colorectal cancer increases with the duration of the disease4.
Systemic Complications
- Liver Disease: PSC is a significant systemic complication associated with UC, increasing the risk of both liver disease and colorectal cancer1 5.
- Extraintestinal Manifestations: These include conditions such as arthritis, uveitis, and skin disorders, which can complicate the clinical course of UC6.
Prognosis of Ulcerative Colitis
The prognosis of UC varies widely among patients and is influenced by several factors, including disease extent, severity at diagnosis, and response to treatment.
Short-term and Long-term Prognosis
- Short-term Prognosis: The initial attack of UC can be severe, but with appropriate treatment, many patients achieve remission. However, the risk of complications remains high during the first few years after diagnosis2 5.
- Long-term Prognosis: Over the long term, the prognosis of UC has improved due to advances in medical and surgical treatments. The overall survival rate has increased, and the risk of colectomy has decreased, although it remains significant for patients with extensive colitis at diagnosis4 10.
Predictors of Outcomes
- Colectomy: Predictors of colectomy include extensive disease at diagnosis, high Pediatric Ulcerative Colitis Activity Index (PUCAI) score, low hemoglobin, hematocrit, and albumin levels, family history of UC, and extraintestinal manifestations1 10.
- Cancer and Mortality: Risk factors for malignancy include longstanding colitis, male sex, younger age at diagnosis, and thiopurine use. Mortality is higher in patients with severe attacks and those diagnosed at an older age1 5.
Impact of Treatment
- Medical Therapy: The step-up approach in medical therapy, starting with 5-aminosalicylates and progressing to corticosteroids and immunosuppressants, has been effective in managing UC and reducing complications6 8.
- Surgical Treatment: Proctocolectomy remains a necessary intervention for approximately 15% of patients, particularly those with refractory disease or severe complications. The type of surgery performed can influence postoperative outcomes and overall prognosis7.
Conclusion
Ulcerative colitis is a complex disease with a variable prognosis. Early identification of prognostic factors and personalized treatment approaches are essential for improving patient outcomes. Advances in medical and surgical treatments have significantly enhanced the prognosis of UC, although challenges remain in managing complications and achieving long-term remission1 4 5 10. Continued research and clinical surveillance are necessary to further optimize the management of UC and reduce the burden of this chronic disease.
Disclaimer
The content presented in this blog is generated by Consensus, an AI-powered academic search engine, and is based on publicly available scientific literature. While every effort is made to provide accurate, up-to-date, and well-researched information, the content is intended for informational and educational purposes only. It does not constitute medical advice, diagnosis, or treatment. Always consult a qualified healthcare professional before making any decisions regarding medical conditions, treatments, or medications. The AI system’s analysis may not cover all perspectives, emerging research, or individual cases, and it is not a substitute for professional expertise. Neither the blog publisher nor the developers of the AI-powered search engine are responsible for any actions taken based on the information provided in this content. Use of this information is at your own risk. Citations to the original scientific studies are included for reference, but these studies should be reviewed in full and interpreted with the guidance of a healthcare or research professional.
If you are experiencing a medical emergency, please seek immediate attention from a healthcare provider.