Check out this answer from Consensus:
Appendicitis is a common and potentially serious condition that requires prompt diagnosis and treatment. Advances in imaging and a better understanding of the disease’s pathogenesis have improved diagnostic accuracy and treatment outcomes. However, clinical assessment remains a cornerstone of diagnosis, and timely surgical intervention is crucial, particularly in complicated cases. Ongoing research continues to refine management strategies, aiming to reduce morbidity and improve patient outcomes.
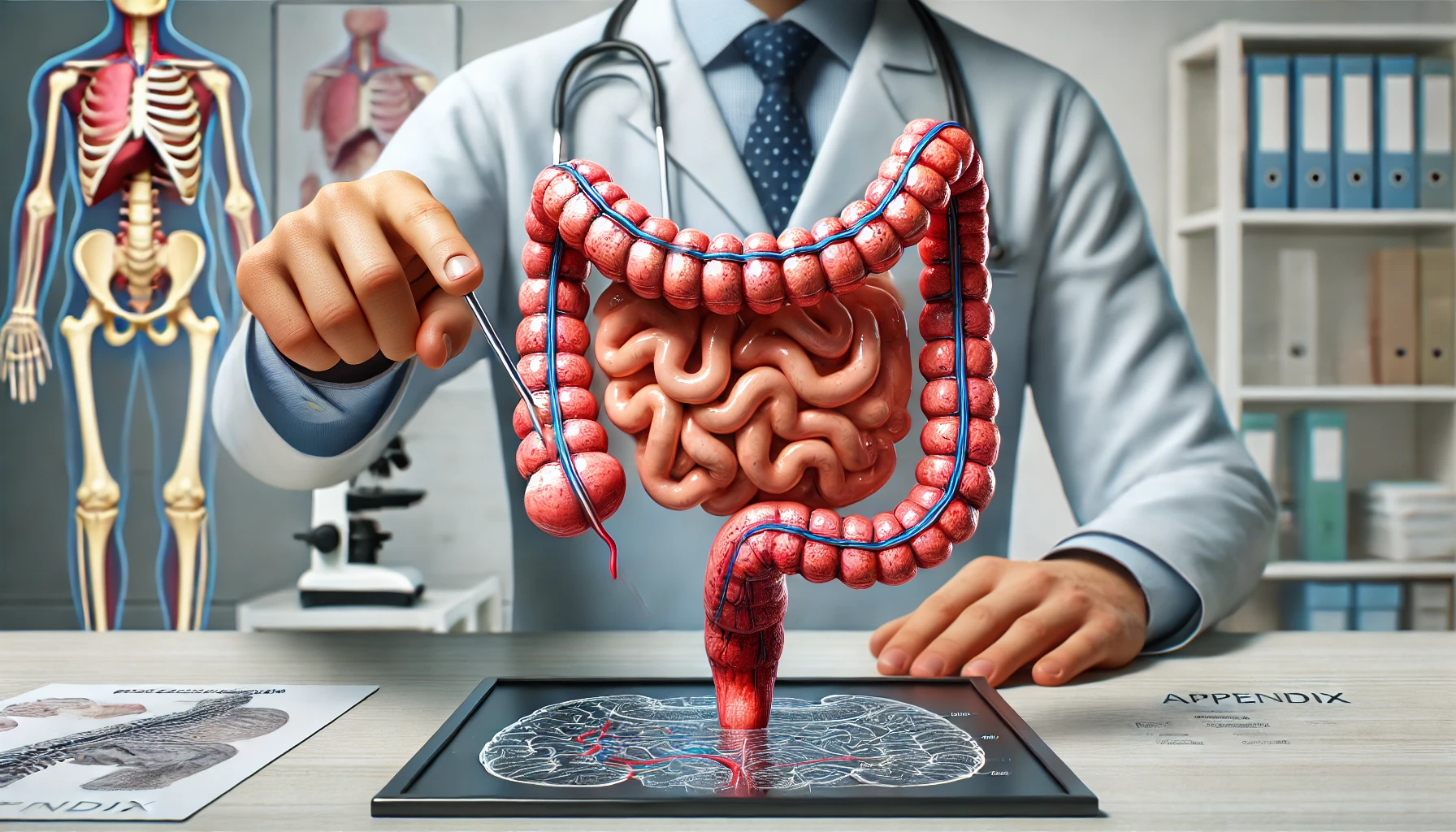
Appendicitis is a common and urgent medical condition characterized by inflammation of the appendix, a small tube attached to the large intestine. It is a significant cause of acute abdominal pain and often requires prompt surgical intervention to prevent complications. This article explores the pathogenesis, diagnosis, and management of appendicitis, drawing on recent research findings.
Pathogenesis
The exact cause of appendicitis remains poorly understood, although it is generally believed to result from obstruction of the appendix lumen, leading to bacterial overgrowth and inflammation1. This obstruction can be due to fecaliths, lymphoid hyperplasia, or foreign bodies. The inflammation can progress to suppuration, gangrene, and perforation if not treated promptly5.
Diagnosis
Diagnosing appendicitis can be challenging due to its variable presentation. Classic symptoms include right lower quadrant pain, nausea, vomiting, and anorexia4. Physical examination often reveals localized tenderness and muscular rigidity in the right iliac fossa. Laboratory tests typically show elevated white blood cell counts and C-reactive protein levels4.
Imaging techniques such as ultrasound and computed tomography (CT) scans are valuable tools in diagnosing appendicitis. Ultrasound is particularly useful in children and pregnant women, while CT scans offer high sensitivity and specificity in adults4 7. Despite these advances, clinical assessment remains crucial, especially in atypical cases1.
Classification
Appendicitis can be classified into uncomplicated and complicated forms. Uncomplicated appendicitis involves simple inflammation without perforation, while complicated appendicitis includes gangrenous or perforated appendicitis3 7. This classification helps guide treatment decisions, with uncomplicated cases sometimes managed conservatively with antibiotics, while complicated cases typically require surgical intervention3.
Management
The standard treatment for appendicitis is appendectomy, which can be performed via open surgery or laparoscopy. Laparoscopic appendectomy is preferred due to its association with less postoperative pain and shorter hospital stays5 9. In some cases, particularly uncomplicated appendicitis, conservative management with antibiotics may be considered, although a significant proportion of these patients may eventually require surgery3 9.
Special Populations
Appendicitis can present differently in various populations. In children, the diagnosis can be more challenging due to atypical presentations and higher rates of perforation5. In older adults, appendicitis is associated with higher morbidity and mortality, often due to delayed diagnosis and treatment2. Pregnant women with appendicitis face unique challenges, as the condition can mimic other pregnancy-related issues, necessitating a high level of clinical suspicion6.